[ad_1]
Over 94% Of Dementia Patients Don’t Recognize Their Cognitive Deficits Because Of This
 Photo by Danie Franco on Unsplash
Photo by Danie Franco on Unsplash
“Mom, you forgot to take your medication again.”
“No, I didn’t. I never forget my pills.”
“But the bottle is still full from last week…”
“You’re wrong. My memory is fine. There’s nothing wrong with me.”
If you’ve had conversations like this with a loved one experiencing dementia, you’re not imagining things—and neither are they, in a way. Over 94% of dementia patients genuinely don’t recognize their cognitive decline, and it’s not because they’re in denial. It’s because of a neurological condition called anosognosia.
This isn’t stubbornness. It’s not pride. And it’s definitely not a conscious choice to ignore reality. Anosognosia is a symptom caused by the same brain damage that causes dementia itself, and understanding it can transform how you care for your loved one.
What Is Anosognosia? (And Why It’s Not Denial)
Anosognosia is a neurological condition that prevents a person from recognizing their own impairment. The word comes from Greek: a (without) + nosos (disease) + gnosis (knowledge)—literally meaning “without knowledge of disease.”
Here’s the crucial distinction: Unlike denial, which is psychological, anosognosia results from changes in the brain that affect self-awareness. People with anosognosia truly believe nothing is wrong, even when symptoms are obvious to everyone else.
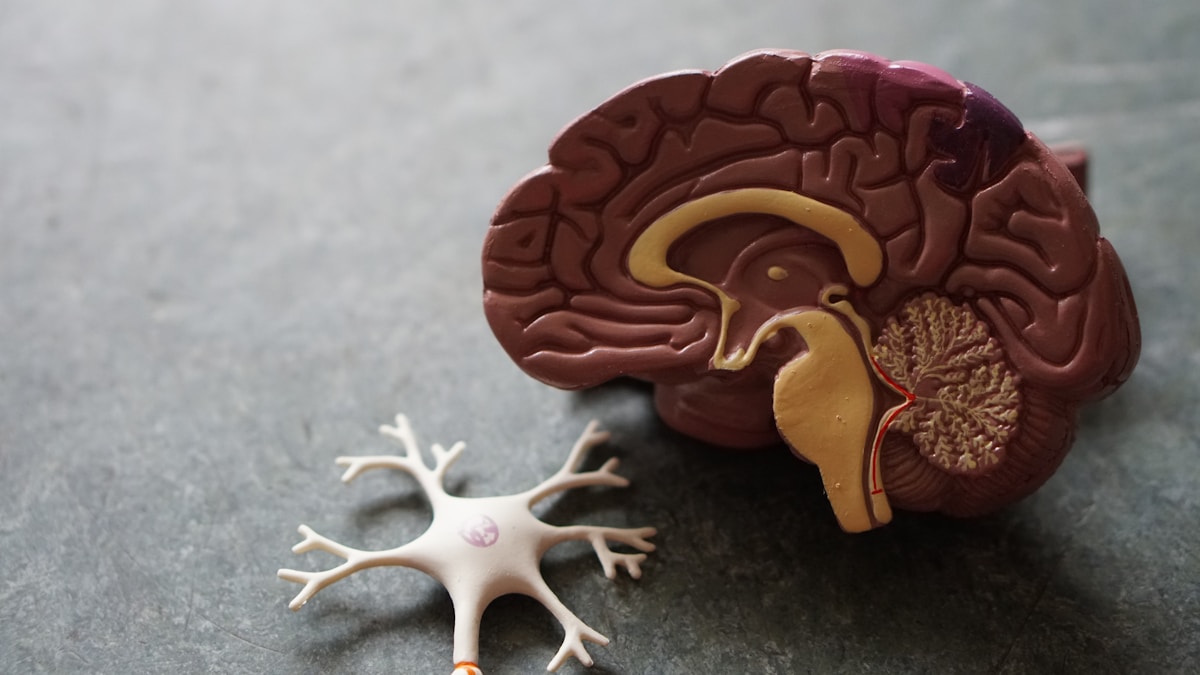 Photo by Robina Weermeijer on Unsplash
Photo by Robina Weermeijer on Unsplash
The Shocking Statistics
Research reveals the staggering prevalence of anosognosia in dementia:
✓ 81% of patients with Alzheimer’s dementia have some form of anosognosia
✓ 94.5% of early-onset dementia cases involve lack of awareness
✓ 60% of patients with mild cognitive impairment (MCI) already show signs of impaired awareness
✓ 50-90% of patients with schizophrenia and 40% with bipolar disorder also experience anosognosia
This isn’t a rare complication—it’s the norm.
The Science: What’s Happening in the Brain?
Understanding the neuroscience helps explain why your loved one isn’t “being difficult”—their brain literally cannot process the information about their deficits.
Brain Regions Affected
Anosognosia typically accompanies damage to specific brain structures, particularly the right parietal lobe, temporoparietal region, thalamus, or basal ganglia. Recent research has identified additional areas involved:
🧠 Prefrontal Cortex: Responsible for working memory, self-monitoring, and organization
🧠 Insular Cortex: Associated with emotional processing, error awareness, and the salience network
🧠 Default Mode Network: Includes connectivity between prefrontal, parietal, and cingulate cortices
🧠 Posterior Cingulate Cortex (PCC): Particularly vulnerable in Alzheimer’s disease
When these areas are damaged, the brain’s “monitoring unit” that mediates conscious awareness of deficits stops functioning properly.
 Photo by Pawel Czerwinski on Unsplash
Photo by Pawel Czerwinski on Unsplash
The Vicious Circle Mechanism
Here’s where it gets really concerning: Anosognosia actually accelerates cognitive decline by preventing patients from being aware of their deficits and implementing strategies to cope with their difficulties, thus fostering a vicious circle of cognitive decline.
Think about it: If you don’t know you have memory problems, you won’t:
- Write things down
- Use medication reminders
- Ask for help
- Seek treatment early
- Follow safety precautions
This creates a downward spiral where lack of awareness worsens the very problems the person doesn’t know they have. For more on cognitive health strategies, check out our guide on B vitamins for healthy brain function.
How Anosognosia Manifests: From Mild to Severe
Anosognosia isn’t an all-or-nothing phenomenon. It exists on a spectrum, and levels and areas of self-awareness vary from person to person. A senior’s lack of insight can be selective or complete.
The Four Levels of Awareness (Anosognosia Rating Scale)
Researchers use a rating scale to measure the level of unawareness:
Level 1: Patients easily admit memory loss
Level 2: Patients admit, sometimes inconsistently, to a small amount of memory loss
Level 3: Patients are not aware of any impairment in memory
Level 4: Patients angrily insist that no memory problem exists
 Photo by Christian Bowen on Unsplash
Photo by Christian Bowen on Unsplash
Domain-Specific Unawareness
Anosognosia may occur in multiple domains, such as the illness in general, specific cognitive deficits, affective changes, or activities of daily living.
A person might:
- Recognize they have trouble finding words but deny having memory problems
- Acknowledge memory issues but refuse to believe they can’t drive safely
- Accept cognitive decline but be unaware of behavioral changes
- Admit some difficulties but be completely unaware of others
Rationalization and Excuses
Dementia patients may rationalize or explain away these situations with a general excuse about age-related forgetfulness or fatigue.
Common rationalizations include:
- “I’m just tired today”
- “Everyone forgets things at my age”
- “You moved my keys—that’s why I can’t find them”
- “The instructions were confusing, not me”
- “I chose not to do that” (when they actually couldn’t)
The Timeline: When Does Anosognosia Develop?
Research shows that amyloid-β burden has been associated with a progressive decline in self-awareness, reaching anosognosia about three years before the dementia stage.
Pre-Clinical Stage
In the very early stages, some people actually have heightened awareness of subtle changes, which can cause anxiety and depression.
Mild Cognitive Impairment (MCI)
60% of MCI patients already show some form of anosognosia. This is often when families first notice the disconnect between what they observe and what their loved one reports.
Alzheimer’s Dementia
81% of patients with Alzheimer’s dementia have anosognosia. The condition typically worsens as the disease progresses.
Predictive Value
Critically, individuals with amnestic MCI with impaired awareness of cognitive decline were 2.86 times more likely to progress to AD within a 2-year time frame than those with intact awareness.
In other words, lack of awareness isn’t just a symptom—it’s a warning sign of faster progression.
 Photo by Andrew Rivera on Unsplash
Photo by Andrew Rivera on Unsplash
The Devastating Impact on Caregivers
If you’re caring for someone with anosognosia, you already know this isn’t just challenging—it’s emotionally exhausting.
Why It’s So Hard
“For dementia caregivers, anosognosia can sometimes be more frustrating to deal with than a loved one’s actual lapses in memory. You witness their abilities changing before your eyes. But how can you convince them that they’re no longer able to safely drive, cook, or handle their finances when they don’t even understand they’re ill?”
Common caregiver challenges:
❌ Safety battles: They insist on driving when it’s clearly unsafe
❌ Treatment resistance: “I don’t need medication—there’s nothing wrong with me”
❌ Medication non-compliance: They forget pills because they don’t believe they need them
❌ Financial risk: They make poor decisions but refuse help
❌ Wandering: They leave home alone, not recognizing the danger
❌ Emotional toll: Constant arguments and accusations of lying or controlling
 Photo by Tim Mossholder on Unsplash
Photo by Tim Mossholder on Unsplash
The Research on Caregiver Burden
Research shows that anosognosia significantly increases caregiver burden, for example by increasing physical symptoms or social isolation. Caregivers for those with both dementia and anosognosia are at greater risk of stress-related health issues compared to those caring for people who retain awareness of their condition.
You’re not just managing memory problems—you’re managing someone who doesn’t believe they have memory problems. That fundamental disconnect makes everything exponentially harder.
For strategies on managing caregiver stress, explore our article on 5 nagging thoughts that keep holding us back in life.
How to Recognize Anosognosia in Your Loved One
Red Flag Behaviors
Watch for these signs that your loved one may have anosognosia:
🚩 Consistent denial of observable problems (not occasional disagreement)
🚩 Anger or aggression when cognitive issues are mentioned
🚩 Blaming others for their mistakes (“You hid my keys”)
🚩 Refusing needed help despite clear inability to manage tasks
🚩 Lack of concern about dangerous situations
🚩 Insisting on independence in clearly unsafe activities
🚩 Rejecting medical treatment they obviously need
The Patient-Caregiver Discrepancy
Diagnosis usually requires clinical assessments to evaluate brain function, observations from caregivers, and brain imaging (MRI or CT scans) that can detect brain changes associated with dementia and assess areas linked to self-awareness deficits.
One common assessment method: comparing what the patient says about their abilities with what caregivers observe. Large discrepancies indicate anosognosia.
 Photo by CDC on Unsplash
Photo by CDC on Unsplash
Evidence-Based Strategies for Managing Anosognosia
There’s no cure for anosognosia, but there are proven strategies to make life safer and less stressful for everyone involved.
The LEAP Method: Your Communication Game-Changer
The LEAP method can help you better communicate with your loved one. It stands for listen, empathize, agree, and partner.
L – Listen: Hear their perspective without immediately correcting them
E – Empathize: Acknowledge their feelings and frustrations
A – Agree: Find common ground, even if it’s small
P – Partner: Work together toward solutions
Instead of: “You can’t drive anymore. You’re not safe.”
Try: “I know you feel confident driving. I’m worried about the roads being busier these days. How about we drive together today?”
Redirection and Distraction Techniques
Instead of directly confronting the person about their lack of awareness, caregivers can use redirection and distraction techniques to avoid potential conflict.
Examples:
- Change the subject when they insist nothing is wrong
- Redirect to a pleasant activity or memory
- Use humor to deflect rather than argue
- Focus on what they CAN do, not what they can’t
 Photo by Sven Mieke on Unsplash
Photo by Sven Mieke on Unsplash
Create a Safe Environment Without Power Struggles
Since a person may not fully recognize their cognitive challenges, it’s important to focus on safety. Gentle home safety measures like reassessing driving abilities, fall-proofing the home, securing firearms, and using medication reminders can help reduce risks and support well-being.
Safety strategies that don’t require acknowledgment of deficits:
✅ Medication management: Pre-fill pill organizers, set alarms, or arrange for delivery
✅ Driving alternatives: Offer to be their chauffeur, arrange rides, or blame car troubles
✅ Financial protection: Set up automatic bill pay, limited-access accounts
✅ Home safety: Install grab bars, remove tripping hazards, improve lighting
✅ Monitoring: Use discreet tracking devices if wandering is a concern
✅ Social engagement: Arrange activities that provide structure and supervision
What NOT to Do
❌ Don’t argue about their deficits: You won’t win, and it damages trust
❌ Don’t use logic to convince them: Their brain can’t process this information
❌ Don’t shame or embarrass them: This only creates defensiveness
❌ Don’t take away independence abruptly: Make gradual changes when possible
❌ Don’t isolate yourself: You need support too
When Cognitive Therapy Can Help
Where anosognosia persists, cognitive therapy can help patients better understand and compensate for their deficit.
While you can’t “fix” the lack of awareness, a skilled therapist can:
- Help develop compensation strategies
- Work on memory aids and routines
- Address anxiety or depression related to subtle awareness
- Support the transition to accepting more help
Important distinction: Anosognosia differs from denial, a psychological defense mechanism that involves avoiding or rejecting information that provokes stress or pain. With denial, the patient may acknowledge a deficit but minimize its consequences and avoid treatments geared to remedy the deficits.
Therapy works better for denial than for anosognosia, but it can still provide valuable support.
 Photo by Natalia Blauth on Unsplash
Photo by Natalia Blauth on Unsplash
Building Your Support Network
Caregivers may want to join support groups or seek guidance from health care professionals experienced in dementia care. A strong support network can provide emotional relief, practical tips and resources to better manage the challenges of caring for someone with anosognosia.
Where to Find Help
🔗 Alzheimer’s Association: Free 24/7 helpline at 1-800-272-3900 and support resources
🔗 National Institute on Aging: Evidence-based information on dementia care
🔗 Local support groups: Connect with others who understand what you’re going through
🔗 Geriatric care managers: Professional guidance for complex situations
🔗 Respite care services: Give yourself necessary breaks
Why Support Matters
Caring for someone with anosognosia is uniquely challenging because:
- You’re managing their reality, not just their symptoms
- You often feel gaslighted by their insistence nothing is wrong
- Others may not understand why “you can’t just explain it to them”
- The emotional burden is compounded by lack of acknowledgment
You need people who get it. Don’t try to do this alone.
The Prognosis: What to Expect
If the cause is a stroke, dementia, or a mass lesion, the prognosis in most cases is poor. If the cause is related to a mental health disorder, the condition leads to difficulty in medication compliance. The overall quality of life is poor.
Progressive Nature
Anosognosia in dementia typically worsens as the disease progresses. The person who initially admits to “small memory lapses” may eventually become angry when any deficits are mentioned.
Impact on Treatment
In some cases, anosognosia may influence treatment decisions, especially when considering disease-modifying therapies (DMTs) for Alzheimer’s disease. Diminished self-awareness can affect how reliably a person reports side effects or follows medical guidance.
The Importance of Early Detection
These findings demonstrating an increase in AD pathophysiology indicate that awareness assessments are a reasonable method to clinically screen individuals for interventions targeting AD pathophysiology in MCI.
Early identification of anosognosia can:
- Predict faster progression to dementia
- Guide treatment planning
- Help families prepare for future needs
- Inform safety interventions before crises occur
For information on cognitive health supplements, read our guide on focus supplements for productivity.
 Photo by Getty Images on Unsplash
Photo by Getty Images on Unsplash
Real Caregiver Perspectives
“My mother has anosognosia—something I didn’t even know existed until I read an article about it a couple of years ago. Just knowing that she lacks the capability to recognize her deficits does make it easier to work with her sometimes because I can strategize with that in mind.”
“If we are to increase understanding and reduce uncertainty experienced by people with dementia, we must fully sink ourselves into dealing with and truly understanding what is experienced and take a more thoughtful approach to their condition.”
The Power of Understanding
Knowledge changes everything. When you understand that anosognosia is:
- Neurological, not psychological
- Caused by brain damage, not character flaws
- Beyond their control
- Not personal attacks on you
You can shift from frustration to compassion, from arguing to adapting, from feeling gaslighted to understanding the reality of brain disease.
Frequently Asked Questions
Is anosognosia the same as denial?
No. Denial is a psychological defense mechanism where someone consciously or subconsciously refuses to accept a diagnosis or health condition. Anosognosia is caused by physical changes or damage in the brain, which impair self-awareness and make it impossible for a person to recognize their condition.
Can anosognosia be treated?
There is no specific treatment for anosognosia, but vestibular stimulation seems to improve this condition temporarily. Management focuses on working around the lack of awareness rather than curing it.
Will my loved one ever acknowledge their dementia?
Possibly, but it’s unpredictable. Some people have moments of clarity or insight, while others never fully recognize their condition. The progression varies by individual.
How do I keep them safe if they won’t admit they need help?
Use strategies that don’t require acknowledgment: automatic systems, environmental modifications, creative reasoning (“The doctor wants me to drive you”), and gentle persistence.
Is anosognosia a sign of worse dementia?
Yes. Research shows that individuals with MCI who have impaired awareness are 2.86 times more likely to progress to dementia within two years. It’s both a symptom and a predictor of progression.
Should I keep trying to make them understand?
No. Repeated attempts to convince someone with anosognosia that they have deficits usually backfires, creating anxiety, anger, and damaged trust. Acceptance and adaptation are more effective.
The Path Forward: Hope and Realistic Expectations
Living with or caring for someone with anosognosia is undeniably hard. There’s no sugar-coating the challenges of managing safety, dignity, and wellbeing for someone who doesn’t believe they need help.
But understanding changes everything.
When you know that your loved one’s brain literally cannot process information about their deficits, you can:
✓ Stop taking their denials personally
✓ Work with their reality instead of against it
✓ Find creative solutions that preserve dignity
✓ Focus your energy on what actually helps
✓ Seek appropriate support for yourself
The Bottom Line
Over 94% of dementia patients don’t recognize their cognitive deficits because of anosognosia—a neurological condition caused by the same brain damage that causes their dementia. It’s not denial. It’s not stubbornness. It’s brain disease.
Your role isn’t to make them see what their damaged brain cannot see. Your role is to keep them safe, maintain their quality of life, and preserve your relationship—all while getting the support YOU need to sustain this challenging journey.
You’re doing harder work than most people will ever understand. Please don’t do it alone.
Additional Resources
🔗 Learn more about dementia care:
- Alzheimer’s Association – Anosognosia Information
- National Institute on Aging – Alzheimer’s Care
- NCBI – Anosognosia Research
🔗 Related articles on cognitive health:
📞 National Resources:
- Alzheimer’s Association 24/7 Helpline: 1-800-272-3900
- Eldercare Locator: 1-800-677-1116
- National Institute on Aging Information Center: 1-800-222-2225
Have you experienced anosognosia with a loved one? Share your story in the comments below. Your experience might be exactly what another struggling caregiver needs to hear today.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Always consult with qualified healthcare professionals for diagnosis and treatment of dementia and related conditions.
[ad_2]