[ad_1]
Healthy Levels Of This Vitamin Increase Success Of Cancer Treatment
 Photo by Michele Blackwell on Unsplash
Photo by Michele Blackwell on Unsplash
When you’re facing a cancer diagnosis, every advantage matters. While most people associate vitamin D with bone health and immunity, groundbreaking research reveals that maintaining healthy levels of this “sunshine vitamin” can dramatically increase the effectiveness of cancer treatment—in some cases nearly doubling the chances of complete tumor response.
The statistics are both alarming and hopeful: up to 91% of cancer patients are vitamin D deficient at the time of diagnosis, yet correcting this deficiency through simple supplementation has been shown to improve treatment outcomes across multiple cancer types. A recent Brazilian study found that breast cancer patients taking just 2,000 IU of vitamin D daily were 79% more likely to achieve complete tumor disappearance after chemotherapy compared to those who didn’t supplement.
If you or someone you love is navigating cancer treatment, understanding the critical role of vitamin D could be one of the most important steps you take in your healing journey. Let’s dive into what the science reveals about this powerful nutrient and how maintaining optimal levels can enhance cancer treatment success.
The Alarming Truth: Most Cancer Patients Are Vitamin D Deficient
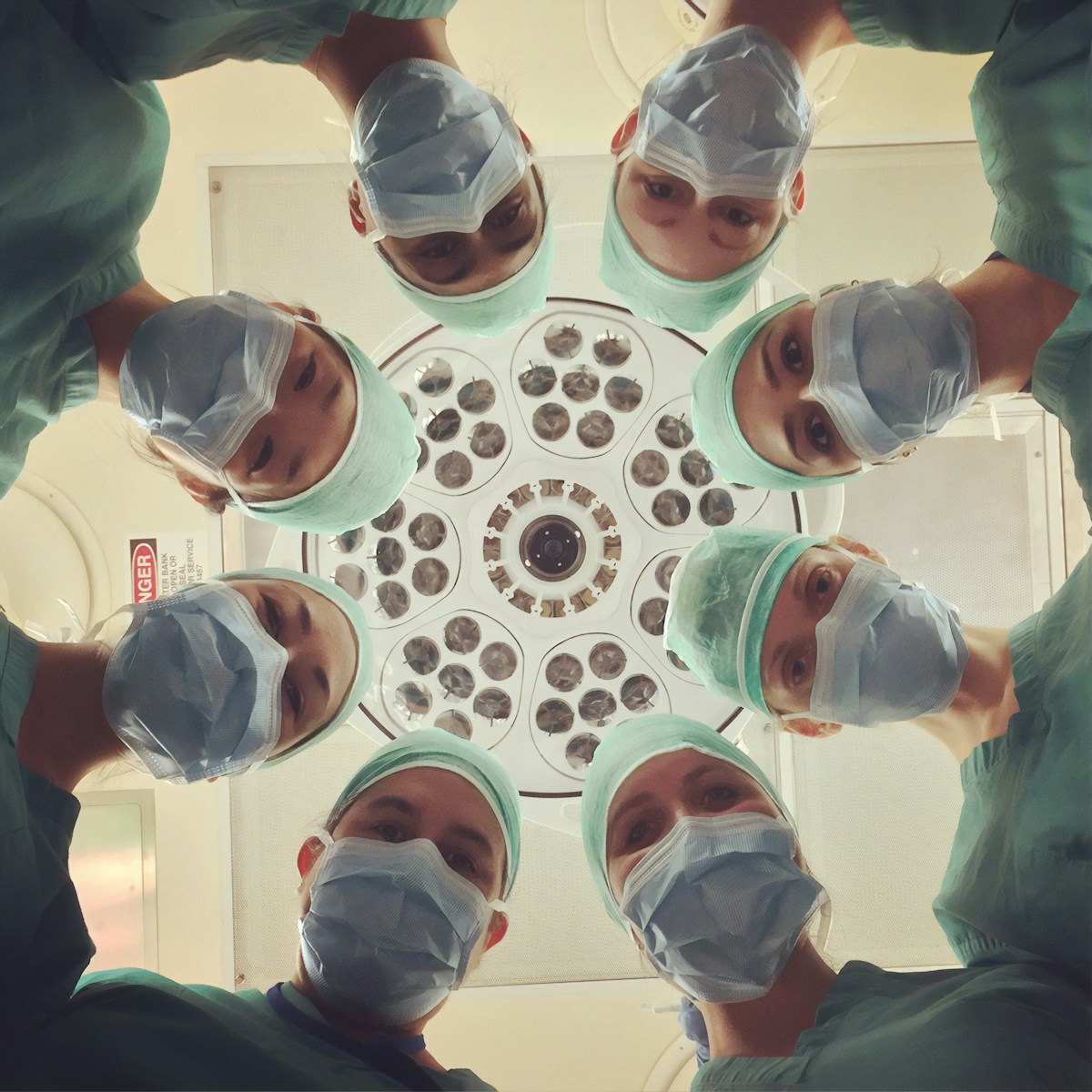 Photo by National Cancer Institute on Unsplash
Photo by National Cancer Institute on Unsplash
Here’s a sobering reality that many oncologists are only now beginning to address: vitamin D deficiency is shockingly common among cancer patients, and this deficiency may be working against treatment success.
Deficiency Rates Are Staggering
Research reveals the scope of the problem:
- 47-91% of cancer patients are vitamin D deficient (<20 ng/mL) at diagnosis
- In one colorectal cancer study, 59% of patients had deficient levels
- A study of breast cancer patients found 85-92% were deficient
- Among advanced cancer patients, 74% had deficiency, with 54% having severe deficiency (≤12 ng/mL)
- 87% of triple-negative breast cancer patients were deficient prior to starting treatment
Even more concerning, in the SUNSHINE trial testing vitamin D in colorectal cancer patients, researchers found that 91% of participants had insufficient vitamin D levels at the start of treatment—and only 9% had sufficient levels.
Why Are Cancer Patients So Deficient?
Multiple factors contribute to widespread vitamin D deficiency in cancer patients:
1. Reduced Sun Exposure Cancer-related fatigue often keeps patients indoors and inactive, limiting natural vitamin D production through sun exposure. Treatment side effects, weakness, and medical advice to avoid sun exposure during certain therapies further compound this problem.
2. Treatment-Related Factors
- Chemotherapy can alter vitamin D metabolism and absorption
- Some cancer treatments affect liver and kidney function, which are essential for vitamin D activation
- Hormone therapies can impact vitamin D levels
- Corticosteroids used alongside cancer treatment increase vitamin D degradation
3. Nutritional Challenges Nausea, loss of appetite, taste changes, and digestive issues during treatment make it difficult to consume vitamin D-rich foods. Weight loss and malnutrition further deplete vitamin D stores.
4. Disease-Related Issues
- Cancer itself can disrupt vitamin D metabolism
- Malabsorption conditions associated with gastrointestinal cancers
- Liver metastases impair vitamin D conversion
- Increased vitamin D consumption by rapidly growing tumors
5. Pre-existing Risk Factors Many cancer patients already had risk factors for deficiency before diagnosis, including older age (decreased skin synthesis), obesity (vitamin D sequestered in fat tissue), darker skin pigmentation, and living in northern latitudes.
 Photo by Dominik Lange on Unsplash
Photo by Dominik Lange on Unsplash
The Breakthrough Research: Vitamin D Improves Cancer Treatment Outcomes
The evidence connecting vitamin D levels to cancer treatment success is becoming increasingly compelling. Multiple studies across different cancer types demonstrate that maintaining adequate vitamin D levels can significantly improve treatment response and survival.
Breast Cancer: 79% Improvement in Complete Response
 Photo by Angiola Harry on Unsplash
Photo by Angiola Harry on Unsplash
The most striking results come from a 2025 study conducted at São Paulo State University in Brazil. Researchers enrolled 80 women over age 45 who were beginning chemotherapy for breast cancer. Half received 2,000 IU of vitamin D daily, while the other half received a placebo.
The Results Were Remarkable:
- 43% of women taking vitamin D achieved complete tumor disappearance (pathologic complete response) after six months of chemotherapy
- Only 24% in the placebo group achieved the same outcome
- This represents a 79% relative increase in complete response rate
What makes these findings particularly significant is that 2,000 IU daily is a relatively low dose—far below the typical 50,000 IU weekly dose used to correct severe deficiency. Yet even this modest supplementation nearly doubled the effectiveness of chemotherapy.
Dr. Eduardo Carvalho-Pessoa, one of the study’s authors and president of the São Paulo Regional Brazilian Society of Mastology, emphasized the accessibility of this intervention: “Vitamin D is an accessible and inexpensive option compared to other drugs used to improve the response to chemotherapy, some of which are not even included in public health systems.”
Colorectal Cancer: 36% Reduction in Disease Progression
 Photo by National Cancer Institute on Unsplash
Photo by National Cancer Institute on Unsplash
The SUNSHINE trial, led by researchers at Dana-Farber Cancer Institute, tested high-dose vitamin D supplementation in patients with metastatic colorectal cancer. All participants received standard chemotherapy (mFOLFOX6 plus bevacizumab), but were randomized to receive either:
- High-dose vitamin D: 8,000 IU daily for 2 weeks, then 4,000 IU daily
- Standard-dose vitamin D: 400 IU daily
Key Findings:
- Patients on high-dose vitamin D had a median progression-free survival of 13 months compared to 11 months in the standard-dose group
- The high-dose group showed 36% lower risk of disease progression or death (hazard ratio 0.64)
- Only patients with sufficient vitamin D levels (achieved in the high-dose group) showed improved outcomes
Importantly, the benefit appeared greatest in patients who:
- Had normal body weight (obesity reduced the effect)
- Did not have KRAS mutations in their tumors
- Achieved vitamin D sufficiency quickly after starting supplementation
Dr. Charles Fuchs, formerly of Dana-Farber and now Director of Yale Cancer Center, stated: “The results of our trial suggest an improved outcome for patients who received vitamin D supplementation, and we look forward to launching a larger trial to confirm these exciting and provocative findings.”
This has led to the ongoing phase 3 SOLARIS trial, which is testing whether adding high-dose vitamin D3 to chemotherapy and bevacizumab can extend progression-free survival in advanced colorectal cancer.
Prostate Cancer: Improved Survival and Reduced Progression
 Photo by Angiola Harry on Unsplash
Photo by Angiola Harry on Unsplash
Research in prostate cancer has yielded encouraging results:
Clinical Trial Results:
- In the ASCENT-1 trial, men with metastatic castration-resistant prostate cancer receiving calcitriol (activated vitamin D) plus docetaxel had improved survival of 24.5 months compared to 16.4 months in the placebo group
- While PSA response rates were similar (63% vs 52%), survival was significantly better in the vitamin D group
- The vitamin D group also experienced fewer adverse events from chemotherapy
Active Surveillance Studies:
- Prostate cancer patients on active surveillance who took 4,000 IU daily for one year showed:
- Decreased Gleason scores (tumor grade improvement)
- Reduced number of positive biopsy cores
- Altered expression of inflammatory genes in tumor tissue
For African American Men: Vitamin D supplementation (4,000 IU/day for 2 months before prostatectomy) showed particularly strong effects in African American men, a population with higher prostate cancer risk and higher vitamin D deficiency rates. The supplementation significantly altered expression of inflammatory genes in prostate tissue.
Head and Neck Cancer: Longer Time to Recurrence
Patients with head and neck squamous cell carcinoma (HNSCC) who received activated vitamin D (calcitriol) for 3 weeks before surgical treatment experienced significantly longer time to cancer recurrence compared to untreated patients.
Cancer Mortality Reduction: 12% with Daily Dosing
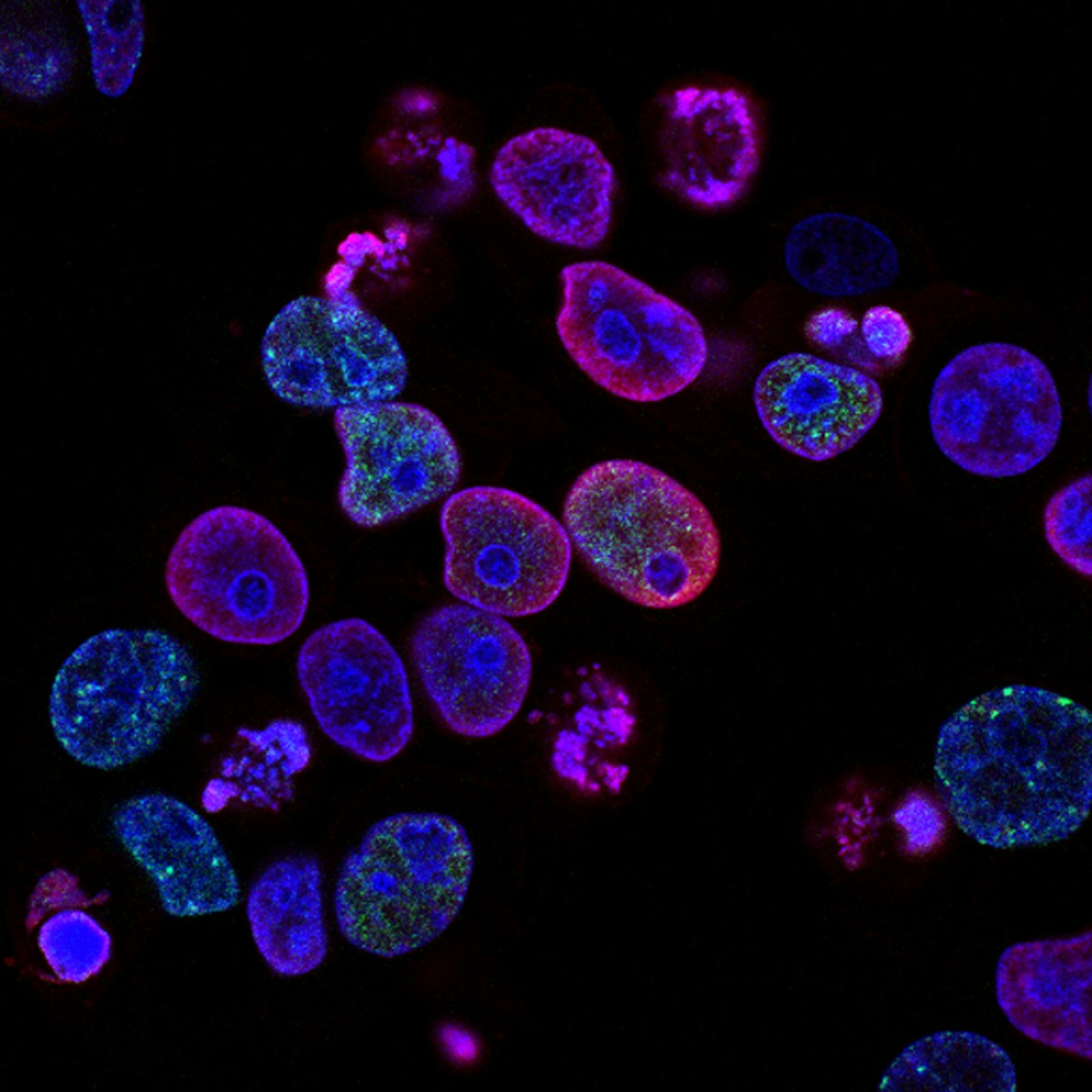 Photo by National Cancer Institute on Unsplash
Photo by National Cancer Institute on Unsplash
A 2023 meta-analysis published in Ageing Research Reviews analyzed 14 high-quality randomized controlled trials with nearly 105,000 participants to determine vitamin D’s effect on cancer mortality.
Critical Finding: Dosing Schedule Matters
When all studies were combined, results were mixed. However, when researchers separated studies by dosing schedule, a clear pattern emerged:
- Daily low-dose vitamin D3 (400-2,000 IU): 12% reduction in cancer mortality (statistically significant)
- Intermittent high-dose vitamin D3 (e.g., 50,000 IU monthly or quarterly): No effect on cancer mortality
The researchers concluded that daily dosing leads to more consistent bioavailability of the active metabolite 1,25-dihydroxyvitamin D, which can inhibit tumor growth more effectively than sporadic high doses.
Lead researcher Ben Schöttker from the German Cancer Research Center explained: “We observed this twelve percent reduction in cancer mortality after untargeted vitamin D3 administration to individuals with and without vitamin D deficiency. We can therefore assume that the effect is significantly higher for those people who are actually vitamin D deficient.”
Prevention Data: 60% Reduction in Cancer Incidence
While this article focuses on treatment, it’s worth noting that maintaining adequate vitamin D levels may prevent cancer in the first place:
- Postmenopausal women taking 1,100 IU vitamin D3 plus 1,450 mg calcium daily experienced a 60% decrease in cancer incidence compared to placebo
- Women with vitamin D levels below 20 ng/mL had a 45% greater risk of developing breast cancer
- Maintaining levels ≥34 ng/mL reduces colorectal cancer risk by 50%
- Maintaining levels ≥52 ng/mL reduces breast cancer risk by 50%
How Vitamin D Fights Cancer: The Biological Mechanisms
 Photo by Louis Reed on Unsplash
Photo by Louis Reed on Unsplash
Understanding how vitamin D enhances cancer treatment helps explain why maintaining adequate levels is so critical. Vitamin D doesn’t just support one aspect of cancer treatment—it works through multiple complementary mechanisms to attack cancer cells while supporting the body’s natural defenses.
1. Inducing Programmed Cell Death (Apoptosis)
Vitamin D triggers cancer cells to undergo apoptosis, a form of programmed cell death that eliminates damaged or dangerous cells without causing inflammation.
How It Works:
- Vitamin D binds to vitamin D receptors (VDR) inside cells, forming a complex that enters the cell nucleus
- This complex activates pro-apoptotic genes like BAX and BAK
- It suppresses anti-apoptotic proteins like BCL-2
- Vitamin D activates caspase enzymes (particularly caspase-3, -8, and -9) that execute the apoptotic program
- It can work through both VDR-dependent and VDR-independent pathways
Importantly, vitamin D-induced apoptosis appears selective for cancer cells. In one study, calcitriol induced apoptosis in tumor-derived endothelial cells but not in endothelial cells from normal tissue, suggesting it preferentially targets cancer-associated vasculature.
2. Arresting the Cell Cycle
Cancer cells divide rapidly and uncontrollably. Vitamin D applies the brakes to this runaway cell division by arresting cancer cells at critical checkpoints in the cell cycle.
Cell Cycle Mechanisms:
- Upregulates p21 and p27: These cyclin-dependent kinase inhibitors stop cells at the G0/G1 checkpoint, preventing entry into the DNA synthesis phase
- Inhibits G1/S transition: Prevents cancer cells from replicating their DNA
- Arrests at G2/M checkpoint: Some cancer types are stopped before cell division
- Downregulates cyclin D1 and c-MYC: Reduces expression of proteins that drive cell division
- Suppresses CDK4 and CDK6: Inhibits enzymes that push cells through the cycle
This cell cycle arrest gives the immune system more time to recognize and eliminate cancer cells, and may make cells more vulnerable to chemotherapy and radiation.
3. Blocking Proliferation Signals
Vitamin D interferes with multiple signaling pathways that cancer cells use to fuel their growth:
Key Pathways Affected:
- Wnt/β-catenin pathway: Vitamin D promotes degradation of β-catenin, reducing its nuclear accumulation and preventing activation of genes involved in proliferation and metastasis
- EGFR (Epidermal Growth Factor Receptor): Vitamin D downregulates EGFR expression, reducing cancer cell response to growth signals
- IGF-1 (Insulin-like Growth Factor) pathway: Suppresses this powerful growth-promoting pathway
- mTOR signaling: Inhibits this master regulator of cell growth and metabolism
- NF-κB pathway: Reduces this pro-inflammatory transcription factor that promotes cancer survival
4. Promoting Cell Differentiation
Cancer cells are typically poorly differentiated—they’ve lost the specialized characteristics of normal cells and exist in an immature, rapidly dividing state. Vitamin D encourages cancer cells to differentiate into more mature, less aggressive forms.
Differentiation Effects:
- Leukemia cells: Calcitriol induces HL-60 leukemia cells to differentiate into mature monocytes
- Breast cancer: Promotes differentiation markers and reduces stem cell-like properties
- Colon cancer: Enhances expression of differentiation markers like E-cadherin
- Prostate cancer: Induces differentiation and reduces aggressive phenotype
More differentiated cancer cells divide more slowly, are less invasive, and may be more responsive to treatment.
5. Inhibiting Angiogenesis (Blood Vessel Formation)
 Photo by National Cancer Institute on Unsplash
Photo by National Cancer Institute on Unsplash
Tumors need to develop their own blood supply to grow beyond a tiny size. Vitamin D disrupts this process through multiple mechanisms:
- Inhibits VEGF (Vascular Endothelial Growth Factor): The master regulator of blood vessel growth
- Reduces endothelial cell proliferation: Prevents the cells that line blood vessels from multiplying
- Decreases tube formation: Blocks the organization of endothelial cells into functional vessels
- Induces thrombospondin-1: An anti-angiogenic protein that inhibits vessel formation
- Targets tumor endothelial cells: Selectively affects cancer-associated vessels while sparing normal vasculature
By starving tumors of blood supply, vitamin D limits their ability to grow and spread.
6. Reducing Invasion and Metastasis
Vitamin D interferes with cancer cells’ ability to invade surrounding tissue and spread to distant sites:
Anti-Metastatic Mechanisms:
- Inhibits matrix metalloproteinases (MMPs): Enzymes that cancer cells use to break down surrounding tissue
- Reduces serine proteinases: Another class of tissue-degrading enzymes
- Increases E-cadherin: A protein that keeps epithelial cells properly attached to each other
- Suppresses epithelial-mesenchymal transition (EMT): Prevents the transformation that allows epithelial cancer cells to become mobile and invasive
- Downregulates SNAIL and SLUG: Transcription factors that promote EMT
- Reduces cancer cell migration: Decreases the ability of cells to move through tissue
7. Modulating the Immune System
 Photo by Fayette Reynolds M.S. on Unsplash
Photo by Fayette Reynolds M.S. on Unsplash
One of vitamin D’s most important anticancer effects is enhancing the immune system’s ability to recognize and destroy cancer cells:
Immune Enhancement:
- Activates dendritic cells: Improves presentation of cancer antigens to T cells
- Enhances T cell function: Improves the cancer-killing ability of cytotoxic T lymphocytes
- Increases NK (Natural Killer) cell activity: Boosts these crucial anti-cancer immune cells
- Modulates macrophages: Shifts them toward an anti-tumor phenotype
- Reduces Treg suppression: Decreases regulatory T cells that normally dampen immune responses and help tumors escape detection
In breast cancer cell studies, vitamin D increased susceptibility to natural killer cell attack by reducing expression of microRNAs that normally protect cancer cells from immune destruction.
8. Enhancing DNA Repair
Cancer is fundamentally a disease of damaged DNA. Vitamin D helps the body repair this damage:
- Upregulates DNA repair genes: Increases expression of genes involved in fixing DNA damage
- Enhances nucleotide excision repair: Improves removal of damaged DNA sections
- Reduces oxidative DNA damage: Increases antioxidant enzymes that prevent DNA damage
- Repairs UV-induced DNA damage: Particularly important for skin cancer prevention
This DNA repair enhancement may help prevent the accumulation of mutations that drive cancer progression and treatment resistance.
9. Reducing Inflammation
Chronic inflammation fuels cancer development and progression. Vitamin D has potent anti-inflammatory effects:
- Suppresses pro-inflammatory cytokines: Reduces IL-6, TNF-α, IL-2, and other inflammatory signals
- Decreases COX-2 expression: Lowers levels of this inflammatory enzyme
- Reduces NF-κB activation: Dampens this master inflammatory pathway
- Modulates prostaglandin synthesis: Reduces inflammatory mediator production
10. Inducing Autophagy (Controlled Cell Degradation)
 Photo by National Cancer Institute on Unsplash
Photo by National Cancer Institute on Unsplash
Autophagy is a cellular recycling process that can either help cancer cells survive stress or lead to their death. Vitamin D can switch autophagy from a survival mechanism to a cell death mechanism:
- Upregulates beclin-1: Increases this autophagy-promoting protein
- Induces DDIT4/REDD1: Inhibits mTORC1, which normally suppresses autophagy
- Promotes cytotoxic autophagy: Triggers autophagy that kills cancer cells rather than helping them survive
- Enhances radiosensitivity: Makes cancer cells more vulnerable to radiation therapy by switching from cytoprotective to cytotoxic autophagy
A recent 2025 study in cervical cancer showed that vitamin D sensitized cancer cells to radiation by inhibiting protective autophagy and increasing apoptosis, mediated through degradation of the Ambra1 protein.
11. Synergizing With Cancer Treatments
Beyond its direct anticancer effects, vitamin D enhances the effectiveness of conventional treatments:
With Chemotherapy:
- In colorectal cancer models, vitamin D combined with 5-fluorouracil showed greater tumor reduction than 5-FU alone
- Combined with metformin, vitamin D reduced early colon neoplasia more effectively than either agent alone
- Mechanisms include enhanced drug uptake, reduced drug resistance, and additive antiproliferative effects
With Radiation:
- Vitamin D-pretreated cervical cancer cells showed increased radiosensitivity
- Mechanisms include reduced protective autophagy and increased apoptosis
- May help overcome radiation resistance
Reducing Drug Resistance:
- Vitamin D can downregulate ABC transporters that pump chemotherapy drugs out of cells
- Improves oxygen delivery to tumors, reducing hypoxia-mediated resistance
- Modulates p53 function, restoring apoptotic responses
Optimal Vitamin D Levels for Cancer Patients
 Photo by Testalize Me on Unsplash
Photo by Testalize Me on Unsplash
Not all vitamin D levels are created equal, especially for cancer patients. While standard medical guidelines define “sufficient” levels differently than what appears optimal for cancer treatment enhancement.
Standard Definitions vs. Optimal Levels
Standard Medical Definitions:
- Deficient: <20 ng/mL (50 nmol/L)
- Insufficient: 20-29 ng/mL (50-74 nmol/L)
- Sufficient: 30-100 ng/mL (75-250 nmol/L)
- Potentially Toxic: >150 ng/mL (>374 nmol/L)
Optimal Levels for Cancer Patients: Many integrative oncologists and researchers recommend higher targets for cancer patients:
- General cancer patients: 40-70 ng/mL (100-175 nmol/L)
- For colorectal cancer prevention: ≥34 ng/mL for 50% risk reduction
- For breast cancer prevention: ≥52 ng/mL for 50% risk reduction
- During active treatment: Aim for the higher end of 50-70 ng/mL
Evidence for Higher Targets
Breast Cancer and Bone Health:
- Women on aromatase inhibitor therapy with vitamin D levels ≥40 ng/mL had significantly less bone density loss (1.7% reduction, p=0.005) compared to those with levels <30 ng/mL
- Women with levels >66 ng/mL experienced significantly reduced aromatase inhibitor-associated joint pain
Colorectal Cancer:
- Meta-analyses show 50% decreased incidence with levels ≥33 ng/mL
- Optimal level for prevention estimated at 36 ng/mL or higher (90 nmol/L)
General Cancer Outcomes:
- Studies consistently show better outcomes at levels >30 ng/mL
- Some research suggests 40-60 ng/mL as the sweet spot for anticancer effects
- The Vitamin D Summit (2009) recommended levels >30 ng/mL (75 nmol/L) for patients with or at risk of cancer
Why Standard “Sufficient” May Not Be Enough
The Institute of Medicine’s definition of sufficiency (≥20 ng/mL) was established primarily for bone health, not for cancer prevention or treatment. This threshold prevents rickets and osteomalacia but may be inadequate for vitamin D’s anticancer effects.
Key Considerations:
- Vitamin D’s gene regulatory effects may require higher levels
- Cancer cells may consume more vitamin D than normal tissues
- Higher levels needed to achieve adequate tissue concentrations
- Individual genetic variations (VDR polymorphisms) affect responsiveness
The U-Shaped Curve Concern
Some studies have shown a U-shaped association between vitamin D levels and certain outcomes—both very low and very high levels associated with increased risk. This has been observed for:
- Pancreatic cancer (very high levels may increase risk)
- Some cardiovascular outcomes
- All-cause mortality in some populations
Important Caveats:
- The “high” levels in these studies (>100 ng/mL) are well above recommended targets
- Much of the U-shaped data comes from single measurements, not sustained levels
- Some cancers (particularly pancreatic) may lose vitamin D receptors as they progress, making supplementation less effective or potentially counterproductive
- Target range of 40-70 ng/mL appears safe and beneficial
Testing Your Vitamin D Level
 Photo by Hush Naidoo Jade Photography on Unsplash
Photo by Hush Naidoo Jade Photography on Unsplash
The only way to know your vitamin D status is through blood testing.
The Correct Test:
- 25-hydroxyvitamin D [25(OH)D]: This is the standard test
- Measures both vitamin D2 and D3
- Reflects your vitamin D status from all sources (sun, food, supplements)
- NOT 1,25-dihydroxyvitamin D (the active form)—this test is NOT used to assess vitamin D status
Testing Schedule for Cancer Patients:
- Baseline: Test at cancer diagnosis before starting supplementation
- Follow-up: Retest after 2-3 months of supplementation to assess response
- Maintenance: Test every 3-6 months during active treatment
- Long-term: Test annually for survivors
Factors That Affect Response to Supplementation:
- Obesity (vitamin D sequestered in fat tissue)
- Malabsorption conditions
- Liver or kidney disease
- Certain medications (corticosteroids, some anti-seizure drugs)
- Genetic variations in vitamin D receptors and metabolizing enzymes
Some people are “high responders” who achieve target levels easily, while others are “low responders” requiring higher doses. Testing is the only way to know.
How to Achieve and Maintain Optimal Levels

Achieving optimal vitamin D levels during cancer treatment requires a strategic approach combining supplementation, diet, and potentially safe sun exposure.
Supplementation: The Most Reliable Method
For most cancer patients, supplementation is the most practical and reliable way to achieve target levels.
Choosing the Right Supplement:
1. Form: Vitamin D3 (Cholecalciferol) vs D2 (Ergocalciferol)
- D3 is superior: More effective at raising and maintaining blood levels
- D3 raises 25(OH)D levels more efficiently than D2
- D3 has longer-lasting effects
- Most studies showing cancer benefits used D3
- Prescription vitamin D is often D2—discuss D3 with your doctor
2. Quality Considerations:
- Choose supplements tested by third-party organizations: USP, NSF International, or ConsumerLab
- Look for pharmaceutical-grade products
- Avoid products with unnecessary additives or fillers
- Check expiration dates (vitamin D degrades over time)
3. Bioavailability:
- Vitamin D is fat-soluble—take with a meal containing fat for better absorption
- Some products come in oil-based soft gels for enhanced absorption
- Micellized or liposomal forms may improve absorption in those with digestive issues
Dosing Guidelines
For Deficiency (<20 ng/mL):
Under medical supervision, typical correction protocols include:
- High-dose correction: 5,000-10,000 IU daily for 2-3 months, then retest
- Alternative: 50,000 IU weekly for 8-12 weeks, then maintenance dose
- May take up to 10 months to fully replenish stores if severely deficient
For Insufficiency (20-40 ng/mL):
- 2,000-5,000 IU daily until target level achieved
- Retest after 2-3 months
- Adjust dose based on response
For Maintenance (≥40 ng/mL):
- 2,000-4,000 IU daily for most people
- Some may need less, others more—testing guides individualized dosing
- Outdoor workers or those with high sun exposure may need lower doses
Important Dosing Notes:
- Daily dosing is more effective than intermittent high doses for cancer benefits
- The upper safe limit set by the National Academy of Sciences is 4,000 IU daily for unsupervised use
- Doses above 4,000 IU should be medically supervised with regular testing
- Vitamin D toxicity is rare but can occur at sustained levels >150 ng/mL
Special Populations:
Obesity:
- May require 2-3 times higher doses to achieve target levels
- Vitamin D is fat-soluble and gets sequestered in adipose tissue
Malabsorption Conditions:
- Crohn’s disease, celiac disease, cystic fibrosis, liver disease
- May need higher doses or alternative delivery methods
On Corticosteroids:
- These drugs accelerate vitamin D metabolism
- Require higher doses and more frequent monitoring
Dietary Sources
 Photo by Caroline Attwood on Unsplash
Photo by Caroline Attwood on Unsplash
While difficult to achieve optimal levels through diet alone, vitamin D-rich foods provide complementary support:
Best Natural Food Sources:
Fatty Fish (highest content):
- Salmon (wild-caught): 570-1,000 IU per 3.5 oz
- Salmon (farmed): 100-250 IU per 3.5 oz
- Mackerel: 345 IU per 3.5 oz
- Sardines: 270 IU per 3.5 oz
- Tuna (canned): 154 IU per 3.5 oz
- Trout: 645 IU per 3.5 oz
Other Animal Sources:
- Cod liver oil: 1,360 IU per tablespoon (but high in vitamin A—use cautiously)
- Egg yolk: 37 IU per large egg (pastured eggs higher)
- Beef liver: 42 IU per 3.5 oz
- Cheese: 12 IU per oz
Mushrooms:
- UV-exposed mushrooms: Can contain 400-800 IU per 3.5 oz
- Regular mushrooms: Minimal vitamin D unless exposed to UV light
- Look for labels indicating “high in vitamin D” or “UV-treated”
Fortified Foods:
- Fortified milk: 100-120 IU per 8 oz
- Fortified plant milk (soy, almond, oat): 100-144 IU per 8 oz
- Fortified orange juice: 100 IU per 8 oz
- Fortified cereals: 40-100 IU per serving
- Fortified yogurt: 80-100 IU per 6 oz
Dietary Reality: To get 4,000 IU from food alone, you’d need to eat approximately:
- 7 servings of wild salmon daily, OR
- 108 egg yolks, OR
- 40 cups of fortified milk
This is why supplementation is essential for achieving therapeutic levels.
Safe Sun Exposure: Proceed with Caution
 Photo by Dawid Zawiła on Unsplash
Photo by Dawid Zawiła on Unsplash
Sun exposure can produce significant vitamin D, but cancer patients must balance potential benefits against very real risks.
The Vitamin D Production Process:
- UVB rays (290-315 nm wavelength) convert 7-dehydrocholesterol in skin to previtamin D3
- Heat isomerizes previtamin D3 to vitamin D3
- 10-15 minutes of midday sun on arms and legs can produce 10,000-25,000 IU
- Skin pigmentation, time of day, season, latitude, and sunscreen use all affect production
Critical Cautions for Cancer Patients:
⚠️ DISCUSS WITH YOUR ONCOLOGIST FIRST
- Some chemotherapy drugs (5-FU, methotrexate, dacarbazine, vinblastine) cause photosensitivity
- Radiation therapy sites remain extra-sensitive long after treatment
- Some targeted therapies increase sun sensitivity
- Immunosuppression from treatment increases skin cancer risk
If Cleared for Sun Exposure:
- Timing: Midday (10 AM – 3 PM) for most efficient UVB, but highest burn risk
- Duration: Start with just 5-10 minutes for light skin, 15-20 minutes for darker skin
- Frequency: 2-3 times per week may be sufficient
- Exposure: Arms and legs, avoiding already sun-damaged areas
- No sunscreen initially (blocks UVB), but apply after the brief vitamin D production window
- Never burn: Any redness means too much exposure
- Avoid face: This area is most prone to sun damage and skin cancer
Who Should Avoid Sun Exposure:
- Anyone on photosensitizing medications
- Those with active radiation therapy or recent treatment
- History of melanoma or other skin cancers
- Fair skin that burns easily
- Multiple atypical moles
- Immunosuppression from treatment
For Most Cancer Patients: Given the complications and risks, supplementation is safer and more reliable than relying on sun exposure for vitamin D.
Combination Approach for Best Results
The ideal strategy combines all three sources:
- Primary method: Daily vitamin D3 supplementation (2,000-5,000 IU) based on testing
- Dietary support: Include fatty fish 2-3 times weekly, choose fortified foods
- Sensible sun (if medically cleared): Brief, intentional exposure during peak UVB times, followed by sun protection
Regular testing every 2-3 months allows you to fine-tune your approach and ensure you’re in the optimal 40-70 ng/mL range.
Vitamin D Interactions and Precautions
 Photo by National Cancer Institute on Unsplash
Photo by National Cancer Institute on Unsplash
While vitamin D supplementation is generally safe, cancer patients need to be aware of potential interactions and precautions.
Medications That Interact with Vitamin D
Corticosteroids:
- Prednisone, dexamethasone, methylprednisolone
- Increase vitamin D metabolism and degradation
- Require higher vitamin D doses
Weight Loss Drugs:
- Orlistat (Xenical, Alli) blocks fat absorption
- Reduces absorption of fat-soluble vitamin D
- Take vitamin D 2+ hours before or after orlistat
Cholesterol-Lowering Drugs:
- Cholestyramine (Questran) and colestipol (Colestid)
- Reduce vitamin D absorption
- Separate doses by several hours
Seizure Medications:
- Phenobarbital, phenytoin (Dilantin), carbamazepine
- Increase vitamin D metabolism
- May need higher doses
Anti-Fungal Drugs:
- Some antifungals affect vitamin D metabolism
- Discuss with your healthcare team
Thiazide Diuretics:
- Combined with high-dose vitamin D may cause hypercalcemia
- Monitor calcium levels if using both
Nutrients That Work Synergistically
Magnesium:
- Required for vitamin D activation
- Deficiency can impair vitamin D metabolism
- Many people are magnesium deficient
- Consider 300-400 mg daily
Vitamin K2:
- Works with vitamin D to direct calcium to bones (not soft tissues)
- May improve safety of higher-dose vitamin D
- Found in fermented foods and supplements (100-200 mcg daily)
Calcium:
- Vitamin D increases calcium absorption
- Cancer patients on certain treatments need adequate calcium for bone health
- Discuss optimal calcium intake with your team (usually 1,000-1,200 mg daily from all sources)
Omega-3 Fatty Acids:
- Some evidence of synergistic anticancer effects
- May enhance vitamin D absorption
- Consider fish oil or algae-based omega-3 supplements
Safety Concerns and Toxicity
Signs of Vitamin D Toxicity (rare, usually at sustained levels >150 ng/mL):
- Nausea and vomiting
- Poor appetite and weight loss
- Constipation
- Weakness and fatigue
- Confusion and disorientation
- Heart rhythm problems
- Kidney stones or kidney damage
- Bone pain
- Elevated blood calcium (hypercalcemia)
Risk Factors for Toxicity:
- Taking extremely high doses (>10,000 IU daily long-term without monitoring)
- Granulomatous diseases (sarcoidosis, tuberculosis)
- Hyperparathyroidism
- Kidney disease
The Safety Window:
- Toxicity is extremely rare at doses <10,000 IU daily
- The therapeutic range of 40-70 ng/mL is well below toxic levels
- Regular testing prevents over-supplementation
Special Caution: If you have hypercalcemia (high blood calcium), do NOT supplement with vitamin D without medical supervision. Some cancers cause hypercalcemia, which would contraindicate vitamin D supplementation until resolved.
Working With Your Healthcare Team
 Photo by Ani Kolleshi on Unsplash
Photo by Ani Kolleshi on Unsplash
Before Starting Vitamin D:
- Get a baseline 25(OH)D test
- Have your calcium level checked
- Discuss any medications or supplements you’re taking
- Inform all members of your cancer care team
Ongoing Monitoring:
- Test 25(OH)D every 2-3 months initially
- Monitor serum calcium, especially at higher doses
- Report any unusual symptoms to your healthcare team
- Keep all providers informed of your supplementation regimen
Vitamin D Across Different Cancer Types
 Photo by National Cancer Institute on Unsplash
Photo by National Cancer Institute on Unsplash
While the majority of evidence supports vitamin D’s beneficial role across many cancer types, the strength of evidence and optimal approaches vary by cancer type.
Strongest Evidence
Colorectal Cancer:
- ✓ Most consistent evidence for prevention and treatment benefit
- ✓ 50% risk reduction with levels ≥33 ng/mL
- ✓ Improved progression-free survival with high-dose supplementation during treatment
- ✓ Reduced colorectal cancer mortality with adequate levels
- Recommendation: Maintain levels 40-60 ng/mL
Breast Cancer:
- ✓ 79% improvement in complete response rate with supplementation during chemotherapy
- ✓ 45% increased risk of development with deficiency
- ✓ Better outcomes with levels ≥40 ng/mL during aromatase inhibitor therapy
- ✓ Reduced bone loss and joint pain at higher levels
- Recommendation: Aim for 50-70 ng/mL, especially during treatment
Prostate Cancer:
- ✓ Improved survival in metastatic disease with activated vitamin D
- ✓ Decreased Gleason scores with supplementation during active surveillance
- ✓ Particularly beneficial for African American men
- ⚠️ Some studies show U-shaped curve—very high levels may not be beneficial
- ⚠️ Advanced prostate cancers may lose vitamin D receptors
- Recommendation: Maintain 40-60 ng/mL; monitor closely
Moderate Evidence
Blood Cancers (Leukemia, Lymphoma, Multiple Myeloma):
- Vitamin D deficiency common (40% in multiple myeloma)
- Shorter time to progression with severe deficiency
- Higher complete remission rates in acute myeloid leukemia with levels >20 ng/mL
- Reduced hospitalization with adequate levels
- Recommendation: Maintain at least 30-40 ng/mL
Head and Neck Cancers:
- Longer time to recurrence with pre-surgical activated vitamin D
- Altered inflammatory gene expression with supplementation
- Recommendation: 40-60 ng/mL
Lung Cancer:
- Mixed evidence; some studies show benefit, others show U-shaped association
- May be more beneficial in early-stage disease
- Recommendation: Maintain 30-50 ng/mL; higher levels warrant caution
Limited or Mixed Evidence
Pancreatic Cancer:
- ⚠️ CAUTION: Some studies show increased risk with very high levels (>100 ng/mL)
- Unclear if this is cause-and-effect or reflects disease processes
- Vitamin D analogs being tested in combination with chemotherapy
- Recommendation: Correct deficiency (aim for 30-40 ng/mL) but avoid very high levels
Melanoma and Skin Cancers:
- Paradoxical relationship: sun exposure increases melanoma risk but also vitamin D
- Higher vitamin D levels associated with better melanoma survival in some studies
- UV exposure for vitamin D not recommended for skin cancer patients
- Recommendation: Supplementation only (not sun exposure); maintain 40-60 ng/mL
Ovarian Cancer:
- Vitamin D deficiency associated with increased risk
- Limited data on treatment outcomes
- Recommendation: 40-60 ng/mL
Thyroid Cancer:
- Some association between deficiency and increased risk
- NCCN guidelines recommend vitamin D screening for thyroid cancer patients
- Limited treatment outcome data
- Recommendation: At least 30-40 ng/mL
General Principles Across Cancer Types
- Correct deficiency first: Even cancers with less evidence benefit from avoiding severe deficiency
- Individual variation: Response depends on vitamin D receptor genetics and other factors
- Timing matters: Daily dosing more effective than intermittent high doses
- Combine with treatment: Vitamin D enhances rather than replaces conventional therapy
- Monitor and adjust: Regular testing guides individualized dosing
- Quality of life: Even without proven survival benefit, vitamin D supports bone health, immune function, and reduces fatigue
Beyond Cancer: Other Health Benefits for Patients
 Photo by Arek Adeoye on Unsplash
Photo by Arek Adeoye on Unsplash
For cancer patients, maintaining adequate vitamin D levels provides benefits that extend beyond tumor control, supporting overall health and quality of life during and after treatment.
Bone Health and Fracture Prevention
Critical for Cancer Patients Because:
- Many cancer treatments (hormone therapies, chemotherapy, corticosteroids) cause bone loss
- Inactivity during treatment weakens bones
- Cancer can metastasize to bones, increasing fracture risk
Vitamin D Benefits:
- Increases calcium absorption by up to 40%
- Maintains bone mineral density
- Reduces fracture risk by up to 20% when combined with calcium
- Essential for patients on aromatase inhibitors, androgen deprivation therapy, or corticosteroids
Optimal Approach:
- Maintain vitamin D levels 40-60 ng/mL
- Combine with calcium (1,000-1,200 mg daily from diet plus supplements)
- Add vitamin K2 (100-200 mcg daily)
- Consider weight-bearing exercise as tolerated
Immune System Support
Vitamin D is crucial for immune function—particularly important during cancer treatment when immunity is often compromised:
- Enhances innate immunity: Increases antimicrobial peptide production
- Regulates adaptive immunity: Modulates T cell and B cell responses
- Reduces infection risk: Studies show lower infection rates with adequate levels
- Supports vaccine response: May improve antibody responses to vaccines
- Modulates inflammation: Reduces excessive inflammatory responses
During cancer treatment, adequate vitamin D levels may help:
- Reduce chemotherapy-related infections
- Support immune-based therapies
- Decrease hospitalization for infections
- Improve recovery from surgery
Muscle Strength and Fall Prevention
Cancer-related fatigue, deconditioning, and certain treatments cause muscle weakness. Vitamin D helps maintain muscle function:
- Improves muscle strength, particularly lower extremity
- Enhances physical performance
- Reduces fall risk by up to 22%
- Supports balance and coordination
- May reduce sarcopenia (muscle wasting)
Particularly Important For:
- Elderly cancer patients
- Those on prolonged bed rest
- Patients receiving corticosteroids
- Anyone at risk for falls
Mood and Mental Health
 Photo by Ksenia Makagonova on Unsplash
Photo by Ksenia Makagonova on Unsplash
Depression and anxiety are common during cancer treatment. While evidence is mixed, vitamin D may help:
- Vitamin D receptors present throughout the brain
- Deficiency associated with increased depression risk
- Some studies show improvement in mood with supplementation
- May enhance serotonin production
- Could improve sleep quality
While not a replacement for mental health treatment, correcting deficiency may support emotional well-being.
Cardiovascular Health
Some cancer treatments (certain chemotherapy drugs, radiation to chest) affect heart health. Vitamin D supports cardiovascular function:
- Helps regulate blood pressure
- Supports healthy endothelial function
- May reduce inflammation in blood vessels
- Plays role in heart muscle function
Optimal range appears to be 40-70 ng/mL; very high levels (>100 ng/mL) may not be beneficial and could potentially increase cardiovascular risk in some studies.
Fatigue Reduction
Cancer-related fatigue is one of the most debilitating symptoms. While not a cure, adequate vitamin D may help:
- Deficiency strongly associated with fatigue
- Correction of severe deficiency can reduce fatigue
- May improve energy metabolism
- Supports mitochondrial function
- Enhances muscle function, reducing physical fatigue
Diabetes and Metabolic Health
Cancer survivors have increased risk of diabetes, and some treatments (steroids) raise blood sugar. Vitamin D supports metabolic health:
- Improves insulin secretion and sensitivity
- May help regulate blood glucose
- Supports pancreatic beta cell function
- May reduce diabetes risk
Important for:
- Patients on corticosteroids
- Those with pre-existing diabetes or prediabetes
- Cancer survivors at risk for metabolic syndrome
Real Patient Perspectives and Clinical Experience
 Photo by Priscilla Du Preez on Unsplash
Photo by Priscilla Du Preez on Unsplash
While research data is compelling, hearing from real patients and clinicians adds valuable context to the vitamin D and cancer story.
From Integrative Oncologists
Dr. Heidi Rula, board-certified family physician and fellowship-trained integrative medicine specialist at Ironwood Cancer & Research Centers in Phoenix, emphasizes vitamin D’s importance:
“Vitamin D is actually one of the most important nutrients in the body that inhibits the development of cancer cells. I generally recommend that my patients get their level somewhere between 40-70 ng/ml. For individuals that are deficient, under a doctor’s supervision, it is recommended to take somewhere between 5,000 to 10,000 IU daily for a few months and have levels rechecked within 3 months. Once your vitamin D level is at an optimal level, most people will need to supplement with 2,000 IU to 4,000 IU a day to maintain good levels.”
Common Patient Experiences
Discovery of Deficiency: Many cancer patients are shocked to discover severe vitamin D deficiency when first tested. Comments from online patient forums reveal:
- “My oncologist finally tested me after I kept asking—I was at 12 ng/mL! No wonder I felt so exhausted.”
- “I thought I was getting enough from my multivitamin (400 IU). Turns out I needed 5,000 IU daily to get into a good range.”
- “After three months on 4,000 IU daily, my level went from 18 to 52 ng/mL and I noticed I had more energy and less joint pain from the AI.”
Response to Supplementation: Patients often report improvements in:
- Energy levels and fatigue
- Joint and muscle pain (especially on hormone therapies)
- Mood and outlook
- Immune function (fewer infections)
- Overall quality of life
Challenges:
- Finding the right dose (individual variation is significant)
- Insurance coverage for testing
- Remembering daily supplementation
- Waiting months to see level changes
- Navigating conflicting advice from different providers
What Oncology Nurses Observe
Oncology nurses, who spend the most time with patients, note:
- Patients with adequate vitamin D often tolerate treatment better
- Fewer delays in chemotherapy cycles due to low blood counts
- Better wound healing after surgery
- Improved physical function and mobility
- Higher energy levels during and after treatment
Words of Caution from Clinicians
Experts emphasize that vitamin D is an adjunct, not a replacement:
- “Vitamin D is not a cure for cancer. It’s one piece of a comprehensive treatment plan.”
- “Don’t delay or refuse conventional treatment to pursue vitamin D supplementation alone.”
- “While we’re excited about the data, vitamin D works best alongside—not instead of—standard cancer therapies.”
- “Test, don’t guess. Taking megadoses without knowing your level can be dangerous.”
Action Plan: Getting Started With Vitamin D Optimization
 Photo by Glenn Carstens-Peters on Unsplash
Photo by Glenn Carstens-Peters on Unsplash
Ready to optimize your vitamin D levels? Follow this step-by-step guide to do it safely and effectively.
Step 1: Test Your Current Level (Week 1)
What to Do:
- Request a 25-hydroxyvitamin D test from your oncologist or primary care physician
- If insurance doesn’t cover it, direct-to-consumer testing is available for $40-80
- Fast not required for this test
- Also request serum calcium level (baseline before supplementation)
What to Ask:
- “Can we check my vitamin D level?”
- “What level should we target given my cancer diagnosis?”
- “How often should we retest?”
Write Down Your Result:
- Date tested: ___________
- Result: _______ ng/mL
- Lab’s reference range: _______
- Target for you: _______ ng/mL
Step 2: Discuss Results With Your Healthcare Team (Week 2)
Key Conversation Points:
- Your current level and degree of deficiency
- Medications you’re taking (check for interactions)
- Appropriate dose to correct deficiency or maintain levels
- Whether you’re on any photosensitizing drugs (affects sun exposure recommendations)
- Retest timing
- Calcium supplementation needs
Questions to Ask:
- “Is this dose safe with my current medications?”
- “Should I take calcium as well?”
- “Are there any reasons I shouldn’t supplement?”
- “When should we retest my level?”
Step 3: Choose Your Supplement (Week 2)
Checklist for Choosing Quality Vitamin D3:
- ✓ Form: Vitamin D3 (cholecalciferol), not D2
- ✓ Dosage: Matches your healthcare provider’s recommendation
- ✓ Third-party tested: Look for USP, NSF, or ConsumerLab seal
- ✓ Form factor: Soft gels, liquid drops, or tablets—choose what you’ll remember to take
- ✓ Free of allergens: If you have sensitivities
- ✓ Reputable brand: From established companies with quality track records
Example Reliable Brands: (Note: This is not an endorsement, just examples)
- Nordic Naturals
- Thorne Research
- Pure Encapsulations
- Garden of Life
- NOW Foods
- Carlson Labs
Where to Buy:
- Pharmacy
- Health food store
- Online retailers (ensure proper storage and expiration dates)
Step 4: Start Supplementation (Week 2)
Dosing Based on Your Level:
If Deficient (<20 ng/mL):
- Typical starting dose: 5,000-10,000 IU daily for 8-12 weeks
- Alternative: 50,000 IU weekly for 8 weeks
- Must be medically supervised at these doses
If Insufficient (20-39 ng/mL):
- Typical starting dose: 2,000-5,000 IU daily
If Sufficient (≥40 ng/mL) but wanting optimization:
- Maintenance dose: 2,000-4,000 IU daily
Best Practices:
- ✓ Take with a meal containing some fat (breakfast with eggs, lunch with avocado, dinner with olive oil)
- ✓ Take at the same time daily (helps remember)
- ✓ Use a pill organizer or phone reminder
- ✓ Keep bottle visible (on breakfast table, by coffee maker)
- ✓ Tell family member or friend for accountability
Step 5: Optimize Your Diet (Ongoing)
Add These Vitamin D-Rich Foods:
- 2-3 times per week: Fatty fish (salmon, mackerel, sardines)
- Daily if possible: Eggs (particularly from pastured chickens)
- Consider: UV-treated mushrooms (can be very high in D)
- Use: Fortified milk or plant milk in smoothies, coffee, cereal
- Occasional: Cod liver oil (1 teaspoon = 1,360 IU, but high in vitamin A)
Sample Day:
- Breakfast: Scrambled eggs, fortified milk in coffee
- Lunch: Salmon salad
- Dinner: (no specific D-rich foods needed)
- Estimated food-based vitamin D: ~800-1,000 IU plus your supplement
Step 6: Consider Complementary Nutrients (Optional but Beneficial)
Magnesium (required for vitamin D activation):
- 300-400 mg daily
- Best absorbed forms: glycinate, citrate, malate
- Take separately from calcium for best absorption
Vitamin K2 (directs calcium to bones):
- 100-200 mcg daily
- Form: MK-7 (longer-acting than MK-4)
- Take with vitamin D for synergy
Calcium (if recommended):
- 1,000-1,200 mg total daily (including diet)
- Best absorbed in divided doses (500 mg at a time)
- Citrate form if taking PPIs or have low stomach acid
- Carbonate form okay if normal stomach acid
Omega-3s (may enhance vitamin D benefits):
- 1,000-2,000 mg EPA+DHA daily
- From fish oil or algae-based supplements
Step 7: Retest and Adjust (Week 10-12)
Retest After:
- 2-3 months of consistent supplementation
- Request both 25(OH)D and serum calcium
Evaluate Results:
- Did you reach your target (40-70 ng/mL)?
- Has calcium remained in normal range?
- Have you experienced any symptoms?
Adjust Dose If Needed:
- Below target: Increase dose by 1,000-2,000 IU daily
- At target: Continue current dose
- Above target (>70 ng/mL): Reduce dose by 1,000-2,000 IU daily
- Much too high (>100 ng/mL): Stop supplementing, retest in 6 weeks
Step 8: Establish Maintenance Monitoring (Ongoing)
Testing Schedule:
- Every 3 months initially until stable at target
- Every 6 months once optimized
- Annually for long-term maintenance
- More frequently if dose changes or new symptoms
Track Your Journey: Keep a simple log:
- Date | 25(OH)D Level | Daily Dose | Notes
This helps you and your healthcare team see trends and make informed adjustments.
Step 9: Watch for Red Flags
Contact Your Healthcare Provider If You Experience:
- Nausea, vomiting, or loss of appetite
- Excessive thirst or urination
- Weakness or fatigue (new or worsening)
- Confusion or mental changes
- Bone pain
- Kidney stones
- Heart palpitations
These could indicate calcium or vitamin D levels too high.
Step 10: Communicate With Your Care Team
Keep Your Team Informed:
- Bring your vitamin D log to appointments
- Report any changes in how you feel
- Discuss test results and dose adjustments
- Ask questions when unsure
- Inform them if you change brands or doses
Integrate Into Cancer Care:
- Make vitamin D status part of routine monitoring
- Include in survivorship care plan
- Continue monitoring even after treatment ends
The Bottom Line: Vitamin D as Part of Comprehensive Cancer Care
 Photo by Peter Herrmann on Unsplash
Photo by Peter Herrmann on Unsplash
The evidence is clear and compelling: vitamin D deficiency is widespread among cancer patients, and correcting this deficiency can significantly improve treatment outcomes. From nearly doubling complete response rates in breast cancer to reducing disease progression by 36% in colorectal cancer, the impact of this simple, safe, and affordable intervention is remarkable.
What We Know:
- 47-91% of cancer patients are vitamin D deficient
- Daily supplementation (not high-dose intermittent) reduces cancer mortality by 12%
- Optimal levels of 40-70 ng/mL appear to offer the greatest anticancer benefits
- Vitamin D works through multiple complementary mechanisms: inducing apoptosis, arresting cell cycles, inhibiting angiogenesis, enhancing immunity, improving DNA repair, and synergizing with conventional treatments
- Benefits extend beyond cancer to bone health, immune function, muscle strength, and overall quality of life
Critical Action Steps:
- Get tested: Don’t guess—measure your 25(OH)D level
- Supplement intelligently: Use vitamin D3, take daily, aim for 40-70 ng/mL
- Monitor regularly: Retest every 2-3 months initially
- Work with your team: Inform all healthcare providers
- Be consistent: Daily dosing is key to benefits
- Combine strategies: Supplementation plus vitamin D-rich foods
- Don’t overdo it: More isn’t always better—stay in the optimal range
- Remember: Vitamin D enhances treatment, it doesn’t replace it
The Most Important Message:
Vitamin D supplementation is not a cure for cancer, and it should never delay or replace evidence-based cancer treatment. However, as an adjunct to conventional therapy, maintaining healthy vitamin D levels is one of the most scientifically supported, accessible, and affordable steps you can take to improve your treatment outcomes and quality of life.
If you’re navigating a cancer diagnosis, talk to your oncology team about testing your vitamin D level today. This simple blood test could reveal a deficiency that, once corrected, may make a meaningful difference in your treatment response and long-term survival.
Your journey with cancer is challenging enough—don’t let vitamin D deficiency be an obstacle to your best possible outcome.
Frequently Asked Questions
Q: Can I take vitamin D if I’m currently in chemotherapy?
A: Yes, in most cases vitamin D supplementation is safe and beneficial during chemotherapy. In fact, the breast cancer study that showed 79% improvement in complete response used vitamin D alongside chemotherapy. However, always inform your oncology team before starting any supplement. They can check for interactions with your specific chemotherapy regimen and monitor your levels appropriately.
Q: How long does it take to correct vitamin D deficiency?
A: This varies by individual and degree of deficiency. With consistent supplementation:
- Mild deficiency (15-19 ng/mL) may correct in 2-3 months
- Moderate deficiency (10-14 ng/mL) typically takes 3-6 months
- Severe deficiency (<10 ng/mL) can take 6-10 months to fully replenish stores
Blood levels start rising within weeks, but it takes time to saturate tissue stores.
Q: Is it better to get vitamin D from sun exposure or supplements for cancer patients?
A: For cancer patients, supplementation is generally safer and more reliable. Sun exposure carries risks of skin damage and cancer, and many cancer treatments cause photosensitivity. Additionally, latitude, season, skin color, and sunscreen use make sun exposure an unreliable source. Supplements provide consistent, measurable dosing without UV exposure risks.
Q: Can you take too much vitamin D?
A: Yes, but toxicity is rare and typically requires sustained levels above 150 ng/mL. The upper safe limit for unsupervised supplementation is 4,000 IU daily. Higher doses should be medically supervised with regular testing. Signs of excess include nausea, weakness, confusion, excessive thirst, and elevated blood calcium.
Q: What’s the difference between vitamin D2 and D3?
A: Vitamin D3 (cholecalciferol) is more effective than D2 (ergocalciferol) at raising and maintaining blood levels. D3 is the form made naturally in your skin from sun exposure and is found in animal sources. D2 comes from plant sources and is often used in prescription vitamin D. For supplementation, choose D3 whenever possible.
Q: Should I take vitamin D with food?
A: Yes, vitamin D is fat-soluble and absorbs best when taken with a meal containing some dietary fat. This could be as simple as eggs, nuts, avocado, olive oil, or cheese. Taking it with a completely fat-free meal reduces absorption.
Q: Will vitamin D interfere with my cancer treatment?
A: Current evidence suggests vitamin D enhances rather than interferes with cancer treatment. Studies show:
- Better chemotherapy response when combined with vitamin D
- Improved radiation sensitivity with vitamin D
- Reduced treatment side effects in some cases
- No negative interactions with most cancer therapies
However, always discuss with your oncology team before starting, as individual situations vary.
Q: My doctor says 30 ng/mL is sufficient. Why do you recommend 40-70 ng/mL for cancer patients?
A: The Institute of Medicine’s definition of sufficiency (≥20-30 ng/mL) was established primarily for bone health, not cancer outcomes. Research specifically looking at cancer prevention and treatment suggests higher levels (40-70 ng/mL) may be optimal for anticancer effects. Many integrative oncologists target this higher range for cancer patients, while still staying well below toxic levels.
Q: I’m on aromatase inhibitors and have terrible joint pain. Can vitamin D help?
A: Yes, studies show women on aromatase inhibitors with vitamin D levels ≥40 ng/mL experience less bone loss and reduced joint pain (arthralgias). One pilot trial found significantly decreased joint pain with levels >66 ng/mL. Many oncologists now routinely check and optimize vitamin D levels in patients on aromatase inhibitors.
Q: Is vitamin D safe for all cancer types?
A: For most cancers, yes. The strongest evidence supports vitamin D for colorectal, breast, and prostate cancers. However, some caution is warranted for pancreatic cancer, where very high levels (>100 ng/mL) in some studies correlated with increased risk. The target range of 40-70 ng/mL appears safe across cancer types, but always discuss your specific situation with your oncologist.
Q: Can I stop taking vitamin D once I reach optimal levels?
A: No, you need ongoing supplementation to maintain optimal levels. Vitamin D levels will gradually decline if you stop supplementing, especially if you have limited sun exposure and don’t eat much fatty fish. Most people need 2,000-4,000 IU daily for maintenance even after reaching target levels.
Q: My vitamin D level is 18 ng/mL. How much should I take?
A: This level of deficiency typically requires 5,000-10,000 IU daily for 8-12 weeks under medical supervision, followed by retesting and dose adjustment. Some doctors prescribe 50,000 IU weekly for 8 weeks as an alternative. Do NOT self-prescribe these high doses—work with your healthcare provider to determine the right correction protocol and monitor your response.
Q: Are there any genetic factors that affect vitamin D levels?
A: Yes, genetic variations (polymorphisms) in the vitamin D receptor (VDR), vitamin D binding protein, and vitamin D metabolizing enzymes can affect how your body responds to vitamin D. Some people are “high responders” who easily achieve target levels, while others are “low responders” requiring higher doses. This is why regular testing is essential—it reveals your individual response.
Q: Should I take vitamin D year-round or just in winter?
A: For cancer patients aiming to optimize treatment outcomes, year-round supplementation is recommended. Even in summer, many people don’t get enough sun exposure (due to indoor lifestyles, sunscreen use, or skin cancer risk), and dietary sources alone are insufficient to maintain therapeutic levels of 40-70 ng/mL.
References and Further Reading
- Dana-Farber Cancer Institute. “High-dose vitamin D shows benefit in patients with advanced colorectal cancer.” 2019.
- Carvalho-Pessoa E, et al. “Effects of vitamin D supplementation on neoadjuvant chemotherapy response in breast cancer.” Nutrition and Cancer, 2025.
- Ng K, et al. “Vitamin D and Colorectal Cancer.” Journal of Clinical Oncology, 2019.
- Trump DL, et al. “Vitamin D and prostate cancer.” Asian Journal of Andrology, 2014.
- Schöttker B, et al. “Efficacy of vitamin D3 supplementation on cancer mortality: Systematic review and individual patient data meta-analysis of randomised controlled trials.” Ageing Research Reviews, 2023.
- Holick MF. “Vitamin D deficiency.” New England Journal of Medicine, 2007.
- Institute of Medicine. “Dietary Reference Intakes for Calcium and Vitamin D.” National Academies Press, 2011.
- National Cancer Institute. “Vitamin D and Cancer Prevention.” Cancer.gov.
- Feldman D, et al. “The role of vitamin D in reducing cancer risk and progression.” Nature Reviews Cancer, 2014.
- Garland CF, et al. “Vitamin D for cancer prevention: global perspective.” Annals of Epidemiology, 2009.
For more information on vitamin D and cancer, visit:
- National Cancer Institute: cancer.gov
- American Cancer Society: cancer.org
- Memorial Sloan Kettering Cancer Center: mskcc.org
Medical Disclaimer: This article is for informational purposes only and is not intended as medical advice. Always consult with your oncologist or healthcare provider before starting any supplement regimen, especially during cancer treatment. Individual needs vary, and what’s appropriate for one person may not be suitable for another.
Have questions about vitamin D and your cancer treatment? Share your experience in the comments below. What has worked for you? What challenges have you faced? Your story could help others navigating similar journeys.
Related Articles You May Find Helpful:
- Understanding Vitamin D Deficiency: Signs, Causes, and Solutions
- Nutrition During Cancer Treatment: What Really Matters
- The Complete Guide to Antioxidants and Cancer
- Supplements to Avoid During Chemotherapy
- Building a Strong Immune System During Cancer Treatment
[ad_2]